About Thyroid Cancer
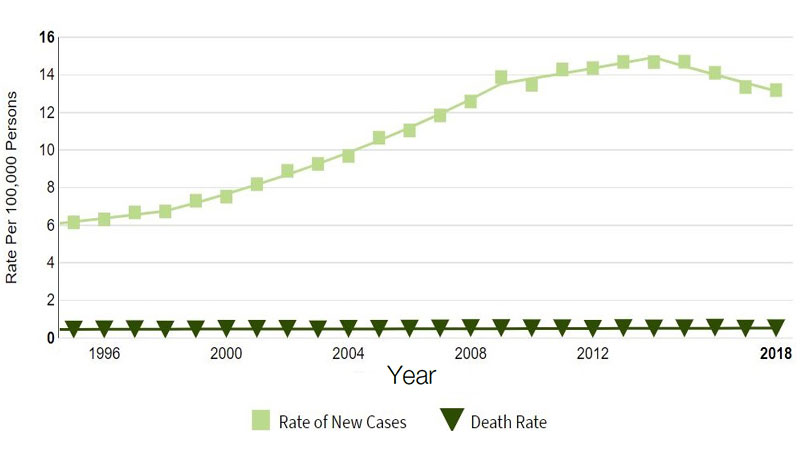
About 1.2% of the population will be diagnosed with thyroid cancer in their lifetime.1 Incidence of thyroid cancer has been increasing faster than any other cancer in the US, tripling in the past 3 decades.2 This rise in incidence is due to enhanced diagnostic techniques that detect small thyroid nodules that may have been missed otherwise and environmental factors, such as exposure to flame retardant dust used in home furnishings. 2-3
As with other thyroid diseases, thyroid cancer is 3 times more prevalent in women than men.2 Women are also more likely to be younger when they develop thyroid cancer, as risk peaks for women in their 40s or 50s, whereas men are usually diagnosed in their 60s or 70s.4
Incidence of thyroid cancer has been increasing faster than any other cancer in the US1
Types of Thyroid Cancer5
The most common types of thyroid cancers – papillary and follicular cancers – develop in the cells that produce the thyroid hormone and resemble healthy tissue. They are sometimes referred to together as differentiated thyroid cancer (DTC).
- Papillary thyroid cancer – The most common form of thyroid cancer and most offen affects people ages 30–50
- Follicular thyroid cancer – Usually affects people over age 50; a rare potentially more aggressive type of follicular thyroid cancer is called Hurthle cell cancer
Other classifications of thyroid cancer:
- Medullary thyroid cancer – Begins in thyroid cells called C cells that produce the hormone calcitonin
- Anaplastic thyroid cancer – A rare, difficult-to-treat cancer that typically occurs in people age 60 or older
- Thyroid lymphoma – A rare form of thyroid cancer that begins in the thyroids immune system cells; typically occurs in older adults
Radioactive iodine (RAI) is a therapy used in the treatment of some thyroid cancers, specifically papillary and follicular thyroid cancer. Other types of thyroid cancers are not susceptible to radioactive iodine intervention.
Thyroid Cancer Diagnosis
Physicians may use one or more procedures to diagnose thyroid cancer, such as a physical exam, biopsy, blood tests, or imaging tests. A common nuclear imaging test called a radioiodine scan may be used to detect thyroid cancer or to show if the cancer has spread in patients already diagnosed. For this test, a patient is given a small amount of radioactive iodine that is absorbed by thyroid cells, which may be seen using a special camera hours later.
Thyroid Cancer Treatment
Most people treated for thyroid cancer have most or all the thyroid surgically removed5; After surgery, patients will need hormone therapy to replace the hormones once produced by the thyroid gland.
Radioactive iodine—also known as iodine-131—may also be given following surgery to destroy remaining thyroid cells and thyroid cancer that may have spread to other areas of the body. This is effective because thyroid cells naturally and selectively absorb iodine, a mineral found in foods such as iodized salt, dairy product, eggs, and some seafood. When radioactive iodine is given to a patient it is absorbed by thyroid cells—including cancer cells—which it then destroys.
Despite treatment, thyroid cancer can return, even if the thyroid has been removed.5 Recurrence most offen occurs in the first 5 years after surgery, but it can come back decades later.5 This may be a result of thyroid cancer cells spreading beyond the thyroid bed area in the neck prior to surgery.5 Post-operative treatment with radioactive iodine has been demonstrated to reduce the risk of recurrence in DTC patients.6

The role of radioactive iodine in the treatment of differentiated thyroid cancer
Jubilant Radiopharma is committed to providing pharmaceutical grade radioactive iodine to enable physicians to accurately diagnose and treat thyroid cancer and help patients achieve and maintain remission.
I-131 Treatment for Differentiated Thyroid Cancer (DTC)
Radioactive iodine (RAI) ablation is the standard of care backed by decades of clinical success for the treatment of DTC.6
Consider this data:
- The 10-year survival rate for DTC patients receiving RAI ablation following total thyroidectomy (surgical removal the thyroid) exceeds 96%7
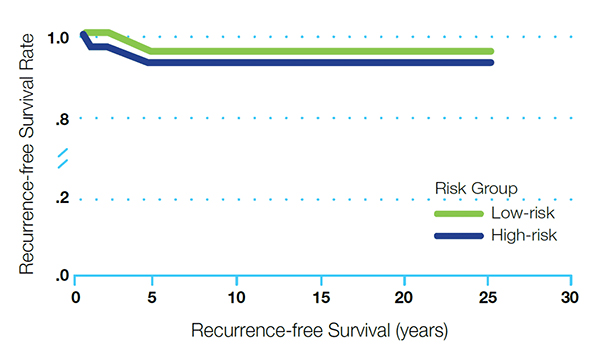
- In DTC, after total thyroidectomy and successful I-131 ablation, high-risk patients did not show a higher recurrence rate than low-risk patients. (see Figure 1)7
Recurrence-free survival in high-risk and low-risk patients (P=0.68)7
A recent study demonstrated that low-risk patients over the age of 45 who receive a dose of greater than 54 mCi have a significantly lower 15-year mortality rate (P=.002) and a higher rate of successful ablation than those patients receiving a lower dose (see Figure 2)8
Low-risk DTC patients =age 45 receiving higher-dose RAI had a lower 15-year mortality rate8*†
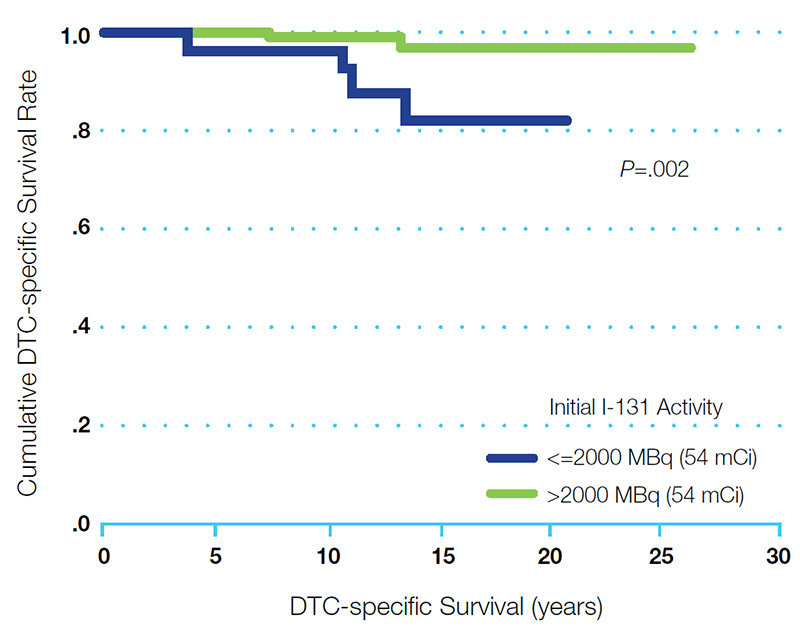
* Low-risk DTC classified as patients with pT1b-T2 tumors without lymph node or distant metastases.
† After complete remission.
In a landmark study involving more than 1,300 thyroid cancer patients showed that, 30 years post-treatment, the cumulative cancer mortality rate in patients who did not receive radioiodine ablation was 3 times that of patients receiving radioiodine ablation (P=0.03)9
Reference:
1. National Cancer Institute. SEER Stat Fact Sheets: Thyroid Cancer. Available at: https://seer.cancer.gov/statfacts/html/thyro.html Accessed on July 7, 2021
2. American Cancer Society. Key statistics for thyroid cancer. Available at: www.cancer.org/cancer/types/thyroid-cancer/about/key-statistics. Accessed on July 7, 2021.
3.Hoffman, K et al, Exposure to flame retardant chemicals and occurrence and severity of papillary thyroid cancer: A case-control study. Environment International, Volume 107, 2017, pgs 235-242
4. American Cancer Society. Thyroid cancer risk factors. Available at: www.cancer.org/cancer/types/thyroid-cancer/causes-risks-prevention/risk-factors. Accessed on July 7, 2021.
5. MayoClinic. org. Thyroid Cancer. Available at: www.mayoclinic.org/diseases-conditions/thyroid-cancer/symptoms-causes/syc-20354161. Accessed on July 7, 2021.
6. Verburg FA, Stokkel MPM, Duren C, et al. No survival difference after successful 131I ablation between patients with initially low-risk and high-risk differentiated thyroid cancer. Eur J Nucl Med Mol Imaging. 2010;37:276–283. pubmed.ncbi.nlm.nih.gov/20091165
7. Siegal E. The beginnings of radioiodine therapy of metastatic thyroid carcinoma: a memoir of Samuel M. Seidlin, MD (1895-1955) and his celebrated patient. Ca Biother & Radiopharm. 1999;14(2):71–79. pubmed.ncbi.nlm.nih.gov/10850290
8. Verburg FA, Mäder U, Reiners C, Hänscheid H. Long-term survival in differentiated thyroid cancer is worse after low-activity initial post-surgical 131I therapy in both high- and low-risk patients. J Clin Endocrinol Metab. 2014;99(12):4487–96. pubmed.ncbi.nlm.nih.gov/7977430/
9. Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med. 1994;97(5):418-28.
DISCLAIMER:
This information is not intended as medical advice. Responsibility for patient care resides with the healthcare professional on the basis of his or her professional license, experience and knowledge of the patient. For full Prescribing Information including indications, contraindications, warnings, precautions and adverse events, please see the appropriate product labeling.

Clinical Resources
Jubilant Radiopharma has made the resources below available for health care professionals who diagnose and treat differentiated thyroid cancer and hyperthyroidism patients: