What is a Pulmonary Embolism?
A pulmonary embolism (PE) is a sudden blockage of an artery in the lung that is usually caused by a blood clot. The blood clot typically originates in the leg and is called deep vein thrombosis (DVT). A PE occurs when the blood clot breaks loose and travels to the lung via the blood stream. Depending on the location and size of the clot, a PE can often cause death in some cases.
The most common symptom of PE is shortness of breath (dyspnea).1 Other symptoms include rapid breathing (tachypnea), bluish skin (cyanosis), fainting (syncope), chest pain, coughing, or coughing up blood.2
A PE is often challenging to diagnose. Approximately half of patients have no obvious symptoms.3 At times, PE symptoms can also resemble those of other conditions, such as pnemonia4 or acute coronary syndrome.5
PE: Common, Yet Often Hidden
Although the exact incidence of PE is unknown, venous thromboembolism (VTE) – which is defined as DVT, PE, or both – affects an estimated 300,000–600,000 individuals in the U.S. each year.6
PE is often fatal:
-
Sudden death is common, affecting up to 25% of people with a PE6
-
10% to 30% of people will die within one month of PE diagnosis6
-
An estimated 5% to 10% of in-hospital deaths are a direct result of PE,7 making it the leading cause of preventable hospital death in the US6
How Is PE Diagnosed?
When a patient is suspected of having a PE, the physician will gather clinical information based on a combination of the patient’s medical history, a physical exam, and diagnostic tests, such as a blood analysis or imaging scan.
Because accurate diagnosis of PE can be difficult, the physician may order a series of tests depending on the patient’s current status, risk factors, and currently available options.
Historically, the most commonly used test to diagnosis PE was pulmonary angiogram, which requires catheter placement through the heart chambers to inject a radioactive tracer into the pulmonary artery. This enables physicians to visualize or detect blockages of blood flow in the lungs by X-ray images. Subsequently, a nuclear medicine test called lung ventilation/perfusion scintigraphy, or V/Q scan, became widely used because it offered a noninvasive way to diagnose PE and could be used in patients who cannot receive iodinated contrast (X-ray dye), such as that used in computed tomographic angiography (CTA).
A V/Q scan consists of 2 parts. In the ventilation part of the scan, a radioactive chemical is inhaled to show how air flows in the lungs. In the perfusion part, a radioactive tracer is injected into a vein in the arm to show blood flow to the lungs. The 2 parts of the study are then compared with each other to evaluate relative rates if ventilation matches perfusion.
Over the past 2 decades, both of these procedures have been overtaken by computed tomography pulmonary angiogram (CTPA)—now the most frequently performed imaging test for PE diagnosis. Using a CT scanner, this test enables radiologists to capture 3-dimensional images of the lungs—as V/Q also does—to detect abnormalities within the arteries. However, a CTPA exposes patients to the same amount of radiation as 100 chest X-rays,8 and should be used with caution for some patients.
A V/Q scan is just as accurate as CTPA. Learn more about the appropriateness of V/Q as compared with CTPA.
Jubilant Radiophamra is committed to providing the radiopharmaceutical products necessary for V/Q scans to allow physicians to accurately diagnose patients suspected of PE and minimize patient radiation exposure.
Use Model for PE Diagnosis9
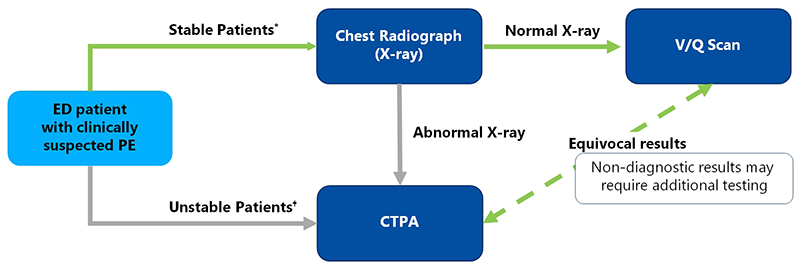
* Suspected PE without hemodynamic instability (e.g., shock or hypotension). † Suspected PE with hemodynamic instability (e.g., shock or hypotension).
Reference:
1. Piazza G, Goldhaber SZ. Acute pulmonary embolism: part I:epidemiology and diagnosis. Circulation. 2006;114(2):e28-32.
2. National Heart, Blood, and Lung Institute. What Are the Signs and Symptoms of Pulmonary Embolism?
http://www.nhlbi.nih.gov/health/health-topics/topics/pe/signs.
3. MedlinePlus. Bethesda (MD): National Library of Medicine (US). Pulmonary embolism; [updated on March 25, 2016]. Available at:
https://www.nlm.nih.gov/medlineplus/pulmonaryembolism.html.
4. Söderberg M, Hedström U, Sjunnesson M, Lärfars G, Jorup-Rönström C. Initial symptoms in pulmonary embolism differ from those in pneumonia: a retrospective study during seven years. Eur J Emerg Med. 2006;13(4):225-9.
5. Kukla P, Dlugopolski R, Krupa E, et al. How often pulmonary embolism mimics acute coronary syndrome? Kardiol Pol. 2011;69(3):235-40.
6. Beckman MG, Hooper WC, Critchley SE, Ortel TL. Venous thromboembolism: a public health concern. Am J Prev Med. 2010;38(4 Suppl):S495–501.
7. Anderson FA Jr, Zayaruzny M, Heit JA, Fidan D, Cohen AT. Estimated annual numbers of US acute-care hospital patients at risk for venous thromboembolism. Am J Hematol. 2007;82(9):777–782.
8. Lin EC. Radiation Risk From Medical Imaging. Mayo Clin Proc. 2010;85(12):1142–1146.
9. Stein, E., et al, Success of a Safe and Simple Algorithm to Reduce Use of CT Pulmonary Angiography in the Emergency Department, AJR: 194, February 2010, pp 392-39790%
DISCLAIMER:
This information is not intended as medical advice. Responsibility for patient care resides with the healthcare professional on the basis of his or her professional license, experience and knowledge of the patient. For full Prescribing Information including indications, contraindications, warnings, precautions and adverse events, please see the appropriate product labeling.