Learn What the Implications Are for Your Practice and Your Patients
The Appropriate Use Criteria (AUC) for Ventilation/Perfusion (V/Q) highlights the value the procedure has in the clinical setting and presents clinical scenarios in which it is most useful. It is a vital and well-accepted resource that will help guide physicians, across specialties, on the appropriate use of V/Q imaging in an accurate, safe, and cost-effective manner; benefiting patients suspected of having acute pulmonary embolism (PE).
Click here to download the AUC for V/Q Imaging in Pulmonary Embolism endorsed by The American College of Emergency Physicians (ACEP)
Click here to watch a video introduction to the AUC document’s salient points from its multidisciplinary authors who address several clinical scenarios for V/Q Imaging in Pulmonary Embolism and its importance to your practice.
What Is an AUC?
AUC are evidence-based and expert consensus-driven guidelines developed to assist medical professionals in making the most appropriate diagnostic and therapeutic decisions when they order and perform a medical procedure. By implementing the AUC, medical professionals will fulfill the requirements of the 2014 Protecting Access to Medicare Act (PAMA) mandated by the Centers for Medicare & Medicaid Services (CMS). Starting January 1, 2018, CMS will require doctors to consult AUC prior to ordering advanced diagnostic imaging services in order to receive Medicare reimbursement. Early adopters of AUC will be eligible to report this use as a high-weighted improvement activity under the Merit-Based Incentive Payment System (MIPS) based on a rule proposed by CMS. CMS has designated qualified Provider-Led Entities (qPLEs)—such as the Society of Nuclear Medicine and Molecular Imaging (SNMMI)—to develop AUCs under the Medicare Appropriate Use Criteria program.
How the AUC for V/Q was developed
The AUC for V/Q was created as a collaborative undertaking initiated by an SNMMI-assembledworkgroup that included experts from the SNMMI, the European Association of Nuclear Medicine (EANM), the American Society of Hematology (ASH), the Society of Thoracic Surgeons (STS), and the American College of Emergency Physicians (ACEP). The wide diversity of the workgroup committee members provided fair balance among a range of interrelated clinical specialties.
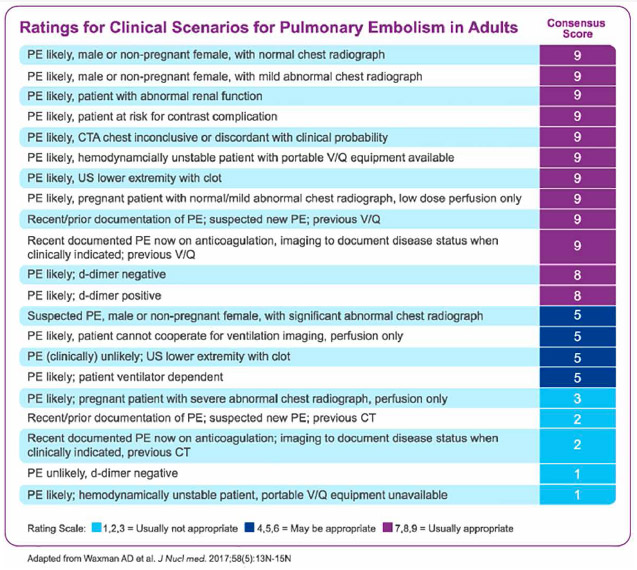
Multiple applications of V/Q imaging were evaluated and rated for appropriateness by the committee. Ratings were based on the consensus of evidence-based literature, as well as expert opinions, and were heavily weighted toward practical clinical scenarios. Based on the AND/UCLA appropriateness method, the workgroup scored each clinical scenario on a scale from 1 to 9 for the use of V/Q:
-
Scores of 7 to 9: Use of the procedure is appropriate for the specific scenario, and generally considered acceptable
-
Scores of 4 to 6: Use of the procedure may be appropriate for the specific scenario; however, more research is needed to clarify and/or support appropriateness
-
Scores of 1 to 3: Use of the procedure is rarely appropriate for the specific scenario, and generally not considered acceptable
The AUC has been published on behalf of SNMMI and will be submitted to CMS for approval.1
Details of AUC for V/Q
The use of V/Q scintigraphy should be considered in many common clinical scenarios in the diagnosis of PE. The AUC guidance for V/Q provides standardization of an evidence- and expert-based diagnostic approach. CMS plans to incentivize physicians to use the AUC through merit-based reimbursement in a proposed rule on the 2018 Quality Payment Program established under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).
The AUC for V/Q is particularly applicable for patients with:
-
Normal or mild abnormal chest radiography
-
Recently documented PE by V/Q scan and suspected new PE
-
Likely PE via ultrasound of lower extremity with clot
-
Recently documented PE by V/Q scan and now on anticoagulation
-
Intravenous radiographic contrast allergy/reactions
-
Renal insufficiencies (eg, ESRD or renal failure)
-
Hemodynamic instability
-
Pregnancy
Professional Recommendations
The ACEP has endorsed the AUC for V/Q, which is significant as emergency physicians are the primary group of physicians that diagnose or rule out PE.
-
The American Thoracic Society recommends V/Q over computed tomography pulmonary angiography (CTPA) in pregnant patients with a normal chest X-ray2, due to the fact CTPA radiation exposure is higher compared with V/Q, posing a substantial risk particularly to the radiosensitive breast tissue of young women or the fetus during pregnancy3
-
The American College of Chest Physicians (ACCP) recommends that for subsegmental PEs with no proximal deep vein thrombosis (DVT), clinical surveillance is suggested over anticoagulation therapy when there is a low risk of recurrent venous thromboembolism (VTE)4
-
Overdiagnosis of small, clinically insignificant PE associated with CTPA has raised concerns about risk of overtreatment and financial implication for further work-up due to these incidental findings.5-7
Additional Resources
Reference:
1. Waxman AD, Bajc M, Brown M, et al. Appropriate Use Criteria for Ventilation-perfusion Imaging in Pulmonary Embolism: Summary and Excerpts. J Nucl Med. 2017;58(5):13N-15N.
2. Leung AN, Bull TN, Jaeschke R, et al. An Official American Thoracic Society/Society of Thoracic Radiology Clinical Practice Guideline: Evaluation of Suspected Pulmonary Embolism In Pregnancy. Am J Respir Crit Care Med. 2011;184(5): 1200–1208
3. Da Silva R, Shah M, Freeman LM. Ventilation-perfusion (V/Q) lung scintigraphy: a long journey to a renewed position of prominence in diagnosing pulmonary embolism. Clin Transl Imaging. 2014;2:369–378..
4. Kearon C, Akl EA, Joseph Ornelas J, et al. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest. 2016;149(2):315–352
5. .Burge AJ, Freeman KD, Klapper PI, Haramati LB. Increased diagnosis of pulmonary embolism without a corresponding decline in mortality during the CT era. Clin Radiol. 2008;63:381–386.
6. Sheh SH, Bellin E, Freeman KD, Haramati LB. Pulmonary embolism diagnosis and mortality with CT pulmonary angiography versus ventilation perfusion scintigraphy: evidence of over diagnosis with CT? Am J Roentgenol. 2012;198:1340–1345.
7. Wiener RS, Schwartz LM, Woloshin S. Time trends in pulmonary embolism in the United States: evidence of overdiagnosis. Arch Intern Med. 2011;171:831–837.